Newswise — Understanding and categorizing the various types of tubulointerstitial responses in acute kidney injury (AKI) may lead to the development of new treatments for the condition, according to a new Yale School of Medicine study published in The Journal of Clinical Investigation on March 17.
The kidneys perform many filtration and excretion functions to keep the body in balance. When kidney function is compromised, AKI can occur.
AKI is a condition in which the kidneys are unable to filter waste from the blood, ultimately leading to long-term kidney damage if not addressed. It is one of the most common conditions for which nephrologists are consulted in hospitals. Despite this, there are very few treatments for AKI, and AKI care has remained mostly the same for the past century.
In the review, researchers categorized AKI tubular epithelial cell injury into four buckets: ischemic, toxic, septic, and primary immune-mediated.
“We are only just starting to think about how immune cells are impacting kidneys after injury, and grouping the injuries helps us better delineate the pathways,” said Megan Baker, MD, a postdoctoral fellow and first author on the paper. “Taking a step back and looking at the literature in a critical way, from the bottom up, helps us better encapsulate what AKI is.”
Using imaging mass cytometry (IMC) on human kidney tissues from the Yale Kidney Biobank, the Cantley Laboratory characterizes protein-level changes in tubular and other cells in the kidney following AKI, and investigates how changes in cell-cell spatial relationships in AKI can inform future therapeutic targets. Baker has led an IMC-based project focused on analyzing ischemic and primary immune-mediated forms of AKI, acute tubular injury, and acute interstitial nephritis, respectively.
By categorizing the injury into these four buckets, we are thinking about how the immune system affects both unique and shared pathways–and hope to identify targets for much more effective therapies in all types of AKI.
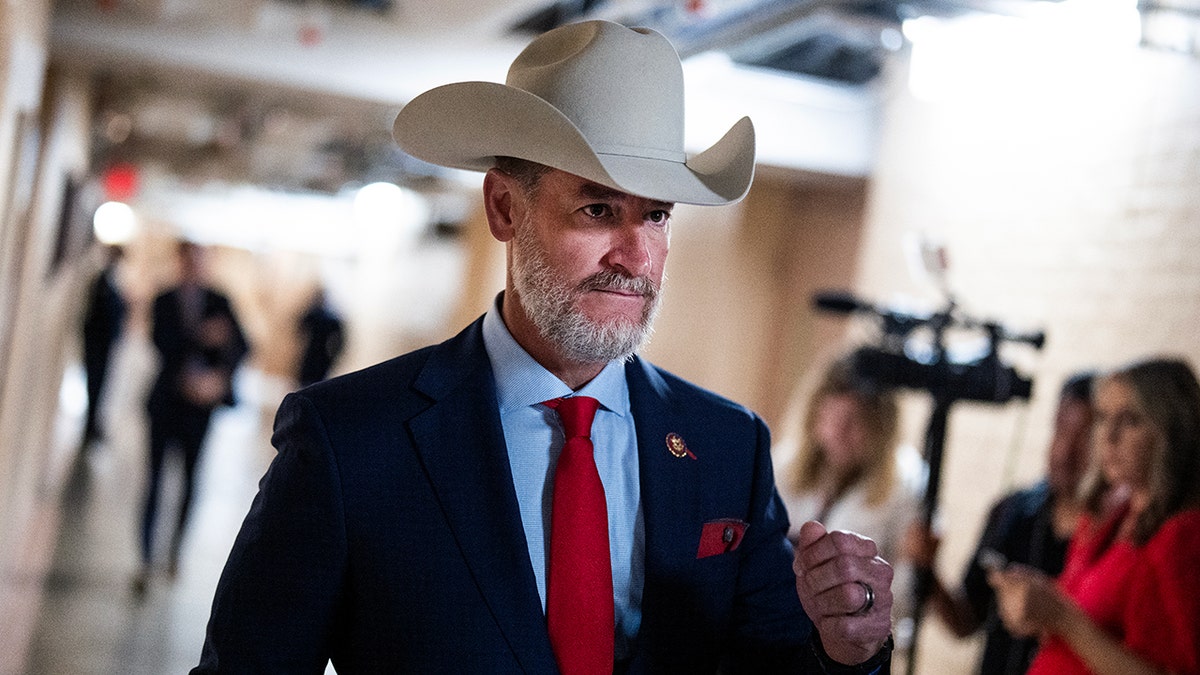
“About eight years ago, I became very interested in translating our research in mouse models of kidney injury to better understand AKI in our patients,” said Lloyd G. Cantley, MD, C.N.H. Long Professor of Medicine (Nephrology) and professor of Cellular and Molecular Physiology, and second author of the paper. “Postdoc Nikil Singh developed the tools to use IMC to analyze biobanked human kidney biopsies, and now Megan has brought this to a level where we’re able to compare normal kidney biopsies to AKI biopsies at a cellular level.”
The review, which provides a framework and guideline for researchers and clinicians to use in thinking about how AKI happens in individual patients, will assist with research and potential treatments, Cantley said.
“There has been a bit of ‘one size fits all’ thinking about how we would develop therapies for AKI, when in fact, the injury mechanisms for different types of AKI can be quite different. So we need to develop therapies that are specific for the type of injury involved and then provide those to the right patients at the right time.” Lloyd said.
The researchers found that in many cases the immune system guides what happens to the kidney after it is injured. They believe they will be able to identify the pathways by which certain immune cells help repair the kidney while other immune cells can harm it.
“Right now, we have only one treatment for AKI, steroids, and that only works for patients with kidney injury due to acute interstitial nephritis. But the treatment is nonspecific,” Baker said. “By categorizing the injury into these four buckets, we are thinking about how the immune system affects both unique and shared pathways–and hope to identify targets for much more effective therapies in all types of AKI.”
Prioritizing the types of therapy or the immune system’s ability to repair the kidney could lead to new insights into improving the outcome of AKI, the researchers said.
Yale’s Section of Nephrology is committed to excellence in patient care, research, and education with the goal for both their faculty and trainees to be national and international leaders in the field of academic nephrology. To learn more about their mission and work, visit Nephrology.